It’s all good when it’s all good, right? When your digestion is working as it should be, you don’t notice anything about it. It’s easy, pain-free and mostly sensationless. For an enormous amount of people, however, this is not the case.
Digestive problems (such as gas, bloating, indigestion, pain, cramping, burning, motility changes and a host of other complaints) are common and among the most cited reasons for missing work or going to your doctor.
Digestive problems cause a lot of heartbreak and prevents us from fully engaging in our lives. Americans pay billions of dollars for over-the-counter and prescription laxatives alone. Acid-blocking medications are among the top three most commonly prescribed drugs, and their recent move to over-the-counter status has skyrocketed their use. Even though digestion is not something we may discuss publicly much, this topic gets a lot of action behind the scenes.
Do you struggle with bloating, gas, constipation, or other digestive issues? We’ve created a FREE guide to healing your gut naturally.
Click here to get your FREE copy of our Digestion Guide!
How Digestion Works

While the physical breakdown of food starts in the mouth, digestion begins as soon as you think about eating. The thought of an incoming meal sends signals from the brain to your gut, priming it by increasing your production of digestive factors and getting your body ready to receive the meal or snack.
As you pop the food in your mouth and begin to chew, your teeth crush it up into smaller pieces, and enzymes contained in the saliva begin to break it down. You swallow, and after a six-second trip down your esophagus, the chewed food is in your stomach.
The stomach is a big blender. Not only does it continue the mechanical breakdown that the mouth has started, it is the mixing place of food, stomach acid, bile and digestive enzymes, all of which cleave the proteins, carbohydrates and fats that you have eaten into their readily absorbable building blocks of amino acids, sugars and fatty acids.
After being reduced to a very soft paste called chyme, the food moves from your stomach to your small intestine. Your small intestine is a rather impressive organ, up to 45 feet long, with so many folds and crypts that if you were to stretch it all out, the surface area would equal that of a tennis court. [tweet_quote]The surface area of your small intestine is about the size of a tennis court![/tweet_quote]
That’s a good thing, considering that the job of your small intestine is to absorb the macronutrients and micronutrients of your food. Your small intestine acts as an intelligent gatekeeper, letting nutrients and beneficial compounds in and keeping harmful compounds and pathogens out. Since the surface area is so large and the potential for exposure to harmful things through what we eat so high, the small intestine is embedded with immune tissue and cells.
Peristalsis is the rhythmical, muscular contraction that propels food down and out and helps you poop regularly. Orchestrated by your “Second Brain” (more on that below), it is responsible for transferring food from your stomach to your small intestine, and from your small intestine to your large intestine. Problems with peristalsis are related to motility – constipation, diarrhea, or both – and are a common reason for distress.
By the time lunch makes it to your large intestine, much of the usable nutrition has been extracted, and your large intestine reabsorbs most of the water. The fiber you have eaten has its time to shine in the large intestine. In addition to helping to keep things moving, fiber is also fuel for your microbiome. The approximately 100-trillion-cell strong colony of beneficial bacteria turn fiber into short chain fatty acids, which the body uses for energy and as anti-inflammatory agents. Keep in mind that you’re not just eating for you, you’re eating for at least a trillion!
Working through the large intestine, the digested food reaches the end of the road and when enough accumulates, you get the urge to defecate. This is the first time that you have had a conscious say in your digestive process since you swallowed your food. Your body does it all for you, under the direction of your Second Brain.
Bottom line: Your brain, mouth, stomach, intestines, pancreas, and gallbladder all play a role in your digestion! This is important to know, because symptoms can give us clues as to which of these parts could be contributing to your digestive problems!
How Your Gut Affects Your Health

There’s good reason to pay attention to your gut even if it doesn’t give you much trouble. Your gastrointestinal system is not only the avenue through which you digest and absorb nutrition, it plays a myriad of other parts when it comes to keeping you in tip-top shape.
Your Gut and Defense
Your gut helps manage defense in three broad ways. First, the stomach and its mighty acid destroy a large number of ingested pathogens and toxicants. Second, the lining of the gastrointestinal tract acts as a smart filter, bringing the good stuff in and keeping the bad stuff out. Last, over two-thirds of the immune system is housed in the gut.
Your Gut and Detoxification
Your body is detoxifying 24 hours a day, seven days a week. It’s not something you have to do yourself or think about. Your gut holds two of the big five organs of detoxification. The liver and the large intestine are responsible for detoxifying and eliminating a mind-boggling array of compounds, both introduced from the external environment and including normal byproducts of your metabolism. The other organs of detoxification – kidneys, skin and lungs – are also influenced by the digestive tract.
Your Gut and Hormonal Balance
Many hormones are assembled, activated, detoxified and excreted via the gut. Up to twenty percent of thyroid hormone is converted to its active form by the activity of the microbiome (the colony of beneficial bacteria residing in your large intestine). Spent estrogens are metabolized by the liver and sent to the large intestine to be pooped out. It’s not an oft thought of cause, but if hormonal imbalances are present with gut disturbance, they can be improved by tuning up digestive health.
Your Gut and Brain
Your digestive system has a brain all of its own, called the enteric nervous system (ENS), or more affectionately, the Second Brain. This is a vast network of nerve cells that are responsible for monitoring and managing every aspect of digestion on a second-to-second basis. There are so many nerve cells that it is equal to that of the spinal cord. It operates independently of your central nervous system – the brain and spinal cord – but takes input from it and gives feedback to it in a bimodal relationship. More and more evidence is suggesting that the state of the gut may have more to do with the state of your central nervous system and even your mental state than was originally thought. Not only is the Second Brain a player in neurological health, the microbiome is too.
Bottom line: The health of your gut is foundational to the health of your body. Your digestive process and how easy or painful it is for you is an indicator of this state. When you understand how it works and the many components that go into it, you can begin to adjust your daily nutrition and lifestyle to promote healthy and pain-free digestion.
5 Signs of Digestive Problems (and How to Heal Them)
Much digestive distress, though it manifests in so many different ways, is caused by similar underlying themes. Eating foods that are not appropriate for you, failing to eat based on symptoms or diagnoses, low digestive ability, an imbalance of the microbiome or frank infection of it, lack of integrity of the intestinal lining, a stressed-out Second Brain, and any combination of these factors underpin much chronic digestive problems.
Keep these factors in mind and the framework outlined for each of them. You can get a lot of relief from digestive problems by following the recommendations described earlier in this guide. This section takes common digestive complaints and gets more specific about how to tackle them.
Bloating

Bloating is one of the most common complaints that people report. Most of us can say that we have felt bloated at one time or another in our lives, but bloating every day, or after every meal, is simply not normal.
You should not have to get into a one-sided wrestling match to peel of your jeans at the end of the day, especially if they so smoothly zipped up in the morning.
If you did a Google search for “causes of bloating,” you might notice that you could compile a list of dozens of reasons. Figuring out the WHY of bloating will shed good light on HOW to de-bloat.
How to De-Bloat

Avoid gas-causing foods
You may bloat because the foods you eat are inherently gas-causing. Beans, broccoli, cabbage, whey, dairy products, protein powders, protein bars, soy, fructose, FODMAPs, inulin, eggs, fake sweeteners and sugar alcohols are common culprits to look out for and minimize.
Support your digestive fire
If you’re not producing enough enzymes, acid or bile, bloating is a natural result as food compounds do not get broken down. Enzymes are particularly useful here, and be sure to see the section above for a more complete discussion on how to improve your digestive ability.
Chew your food
Eating on the run, scarfing down a sandwich on the way to your car, or slamming down a protein shake standing by the sink doesn’t give your body much time to get into a nice, relaxed state to support optimal digestion. Eating quickly and talking with your mouth full introduces a lot of extra air that eventually has to escape. Sit when you eat, slow down, and chew your food until it is a soft paste. This will help decrease gas and bloating and cut down on overeating, too.
Support your microbiome
Rapid bloating after meals is a common symptom of SIBO (small intestine bacterial overgrowth). Bloating that increases during the day and comes with distension is also a sign of SIBO and other forms of dysbiosis. Consider implementing some of the microbiome-boosting strategies, and if those do not help, it’s time to get tested.
Use carminative herbs
Carminative is another way to say gas-reducing. These herbs often are available as tea, singly or in blends. Chamomile, fennel, anise, peppermint and caraway are all excellent choices, and you can determine which ones you enjoy most. If tea is not your thing, they are available in drops or capsules that can be taken after meals.
Consider encapsulated peppermint oil
Encapsulated peppermint oil is a stronger version of peppermint tea. It helps to reduce gas and bloating and relieve the spasms and cramping associated with it. Peppermint should not be used by those with GERD, heartburn or reflux because it can worsen symptoms. For everyone else, it’s wonderful.
Bottom line: Getting clinical in your approach to examining the common root causes of gas and bloating will assist you in narrowing down what is causing the issue for you.
Constipation

If you have less than three bowel movements per week (some would argue less than one per day), feel as if you are not quite “done” at least 25% of the time, feel as if there is an obstruction at least 25% of the time, if stool is hard 25% of the time, or if you need to use an instrument or enema or some other form of help at least 25% of the time – you’ve got constipation.
Constipation is very common and expensive. Americans spend $800 million plus on over-the-counter laxatives. As with bloating, there are many themes to look at, including the foods you are eating, your ability to digest, the health of your microbiome and the flexibility of your Second Brain.
When it comes to tackling constipation and regulating your motility, there are several factors to look at.
How to Relieve Constipation

Eat more fiber AND stay hydrated
When it comes to constipation, fiber can be a tricky issue. One: not all fibers are the same. Two: in many cases, constipation is not the result of a fiber deficiency, and when we begin to load up on Metamucil because our doctor said so, it can slow us down even more, particularly if we are dehydrated!
Fiber adds bulk and volume to the stool, which actually helps our Second Brain push it along and out. This ONLY works, however, if we are well hydrated. So, if we are indeed fiber-deficient, the very first order of business is to begin to increase our water.
Now, my very favorite form of fiber is the type found in vegetables. If you are getting in non-starchy veggies, you are also getting a bit of water to go alongside your fiber and helping the entire process move right along. [tweet_quote]Veggies add both fiber and water to your digestive system.[/tweet_quote]
Eat at least four cups of vegetables daily, at a bare minimum. Not only are the veggies providing fiber and water, they are also providing minerals (also key for regularity), vitamins, antioxidants and a variety of healthy phytochemicals. Veggie intake is hugely important.
Some are interested in supplemental fiber, and for that, the gentlest one on the block is acacia. Like probiotics, fiber is something that you want to start at low amounts and slowly increase over time to not exacerbate symptoms. Start with 1/2 teaspoon in 8 ounces of water, and every 3-4 days increase this amount by 1/4-1/2 teaspoon until you are doing 2-3 teaspoons in 8-10 ounces of water twice daily.
Eat healthy fats
Intake of healthy fats helps keep the bowel lubricated and thus things moving along.
Choosing high-quality fats is of utmost importance, not just for digestion but for overall health and wellness. In addition to being a lubricant, fats are key for building hormones, cellular communication and nerve signaling/transduction. They are also pivotal in the production of the inflammatory and anti-inflammatory compounds your body produces, and you want a correct balance of both for wound healing (to fight infection and to clean up the mess left) and to be able to quench free radicals and other inflammatory compounds as well.
A mix of fats, of animal and plant origin, is ideal. When it comes to animal fats, buy the absolute best that you can afford, focusing on fish that are wild-caught, meats that are grass-fed, and chicken/poultry that is pastured.
In the plant kingdom, the easiest and safest options to stick with for cooking are extra virgin olive oil (look for labels that say “100% olive oil” – otherwise you may be getting a blend cut with canola or soy oil), coconut oil and avocado oil. Oils to stay away from are canola, soy and anything labeled “vegetable oil.” Seed oils are best consumed raw, as in a salad or other veggies.
Avocado, nuts and seeds and their butters, coconut and coconut products, egg yolks, fatty fish (salmon, mackerel), and fattier cuts of meat (ribeye, chuck) are all good sources of fats.
Add minerals and electrolytes
Minerals and electrolytes help maintain appropriate hydration levels and help keep the bowel open and flexible so that overall, movements are easy and painless.
Magnesium (more on magnesium below), potassium, calcium, selenium, sodium and zinc all work in harmony to achieve this state of fluid balance and open bowel.
Veggies and fruits are loaded with electrolytes and minerals, and thus can exert their beneficial effects that way. Certain medications readily deplete minerals and electrolytes, particularly ones that regulate blood pressure and cardiovascular function, but antibiotics, antidepressants and birth control are culprits too. A complete mineral complex or a multivitamin that has a multi-mineral complex embedded in it can be beneficial for those who do not or cannot eat a wide variety of veggies or fruits, or for those taking these medications.
Try magnesium ascorbate (MA) powder
First thing in the morning, drink 10 ounces of room temperature water with a squeeze of lemon and 1/4 teaspoon magnesium ascorbate powder. This is a vitamin C powder buffered by magnesium. It is a very gentle laxative and bowel re-trainer, without the risk of dependency like some of the herbal laxatives. The trick with the MA powder is to find the right dose. If this dose does not stimulate a bowel movement within an hour, slowly increase it by 1/8 teaspoon every several days until you hit the right dose.
Establish a bathroom routine
Your bathroom should be soothing and pleasing to the senses. Using aromatherapy, candles and fun wall coverings, art or paint can all help create a relaxing atmosphere. Each morning, sit on the toilet and empty your mind. Focus on your breath. Sit for 5-10 minutes each morning, whether you have a bowel movement or not.
Bring a small foot stool into the bathroom
It doesn’t have to be special or fancy or a Squatty Potty, but as you sit on the toilet, put your feet up on the foot stool. Your knees should be above the level of the hips. This puts your anatomy in the right place for a smooth bowel movement. Use the foot stool every single time you sit down for a bowel movement, whether you go or not.
Utilize perineal acupressure daily
Stay with me here. Research suggests that daily perineal acupressure can reduce constipation by up to 80% over a 4-week period. This is an enormous improvement. The acupressure point to press is the space between the anal opening and the genitals (your perineum). As part of your bathroom routine, apply firm but comfortable pressure there for 60 seconds each morning when you are sitting and breathing.
Go for a daily walk
Gentle movement, in the form of a leisurely walk, helps to retrain the Second Brain and the body and is a secret weapon against chronic constipation. The walk should have an element of mindfulness to it. Try to immerse yourself in the sensations: feel the sun and air on your skin, notice the sounds around you. When your mind wanders, bring it back to those immediate sensations. Aim for 30 minutes daily.
Around bedtime, take 400-500mg of magnesium glycinate
This gently helps dilate and retrain the bowel and helps to set you up for a bowel movement in the morning. You can increase by 200mg every several days until you achieve movement. Magnesium is very safe to take in high doses, with the worst side effect being loose stool. Magnesium is good for cardiovascular function, blood pressure, tight muscles and sleep. It covers a lot of bases. Pairing magnesium ascorbate powder in the morning with magnesium glycinate in the evening helps with even the toughest constipation.
Consider triphala in tough cases
This herbal formula (a mixture of three herbs) helps to stimulate both digestive fire and peristalsis.
Bottom line: Constipation is a common and costly complaint. We now understand that constipation is not due to a simple lack of fiber – there can be multiple causes, including nutrition, the health of the gut bacteria, the flexibility of the Second Brain, uncompensated stress and a sedentary lifestyle.
Diarrhea

Diarrhea can be categorized as infectious or noninfectious. Infectious diarrhea means you’ve got some pathogen and your body is doing its best to get it out. Infectious diarrhea typically resolves on its own or is something you receive an antibiotic for. Antibiotics, of course, can create diarrhea as well.
Non-infectious diarrhea implies that there are no pathogens or bad bugs responsible and that there is some other cause. Diarrhea can be a predominant symptom of IBS-D, colitis and IBD.
As with bloating and constipation, uncovering the reasons why diarrhea is present will shine the light on how to approach it. Look at your nutrition, your digestive ability, the health of your microbiome and digestive lining, and most importantly, your Second Brain.
Get a stool test
Any diarrhea that lasts longer than two weeks deserves a thorough evaluation. A stool test can rule out frank pathogenic infections like giardia, C. diff, clostridium and harmful E. coli. A comprehensive digestive stool analysis (CDSA, see above in microbiome section for more complete information) can also determine your levels of beneficial bacteria, markers of inflammation, and if you are spilling fats, proteins or fibers into the stool, all of which will help shape treatment.
Buy non-GMO products
Stephanie Seneff, a researcher at MIT, is studying the effects of Roundup (glyphosate) on human and bacterial health. Roundup is typically sprayed on genetically modified, Roundup Ready crops (wheat, sugar, and soy being the most common). Seneff illustrated that Roundup can interfere with the serotonin metabolism and signaling of bacterial cells. Chronic, non-infectious diarrhea often accompanies high serotonin or serotonin excessive states. Serotonin helps initiate the wave of peristalsis – the muscular contraction that moves food down and out – and diarrhea is peristalsis gone awry. While the safety of Roundup and GMO crops has not been fully elucidated in humans, chronic diarrhea sufferers would do well to avoid these items.
Take a probiotic
Probiotics help regulate bowel motility and calm the Second Brain. They are particularly important if you have taken antibiotics recently or if antibiotics preceded your diarrhea. Aim for 50-100 billion CFUs of a probiotic that contains Bifidobacterium breve, longum and infantis at a minimum.
Consider acacia fiber
It’s not just for constipation. Acacia is very gentle and a great stool binder, helping to add bulk and consistency. Start with 1/2 teaspoon in 8 ounces of water, and every 3-4 days increase this amount by 1/4-1/2 teaspoon until you are doing 2-3 teaspoons in 8-10 ounces of water twice daily.
Take zinc and zinc carnosine
A zinc lozenge containing 5mg zinc can be taken two to three times daily to help slow you down. Zinc carnosine can quell diarrhea and will also help mitigate the local irritation and inflammation that can come with it.
Avoid raw foods, for now
Raw foods are harder for your body to break down and more irritating to the lining of your digestive tract. You may notice more undigested food in the stool when you are eating raw items. Focusing on warm, cooked foods and broths is not only soothing, but broths will help replenish fluids and electrolytes lost from diarrhea.
Bottom line: Fast transit time not related to infection/food poisoning can have several different causative factors, all of which should be explored. The health of the lining of the intestine should always be attended to in cases of chronic diarrhea.
Low Stomach Acid

Your stomach acid serves multiple functions. It helps break down protein and absorb certain vitamins and minerals (think folate, iron and B vitamins). Stomach acid acts as defense against bad bacteria and other bugs and viruses that can make you sick, and maintains an appropriate pH throughout the entire system.
Low stomach acid is most common in those who take acid-blocking medications, the chronically stressed, and the elderly.
Symptoms of low stomach acid include excess belching, bloating, difficulty digesting proteins, anemia (both iron and B vitamin deficiency), frequent urinary tract, vaginal or upper respiratory tract infections, and reflux.
What to Do If You Have Low Stomach Acid
It is possible to be tested for low stomach acid through the Heidelberg test, although not many doctors perform this test. Based on your symptoms and your history, your health care provider may recommend a trial of supplemental acid (known as Betaine HCl) taken with meals to see if it improves symptoms.
If you have gastritis or an active ulcer, you should NOT take supplemental acid.
Bottom line: Your stomach acid helps break down your food, keep your gut running smoothly, and protect you from illness. Symptoms of low acid can be uncomfortable and are often reversed with Betaine HCl supplementation, but don’t ever supplement if you have an ulcer or gastritis.
Gut Infections and Parasites
You have learned that dysbiosis is a major factor in much chronic digestive distress and has implications for disease not limited to the gut. Sometimes, there is more than just an imbalance present in your microbiome – there is frank infection. A pathogenic bacteria, yeast or parasite is on board.
How to Get Rid of a Gut Infection or Parasites

Get a stool test
If you suspect an infection, it is imperative that you get a stool test. A CDSA test (explained in depth in the microbiome section above) will not only pinpoint which bad guys are present (or if they are not present), it will also determine exactly what pharmaceutical and natural antimicrobials they are sensitive to. It will tell you exactly what you need to kill them, and that saves you a lot of time, money and guesswork.
Go low-FODMAP
For the course of your treatment, choosing foods that are low on the FODMAP scale (see below in the nutrition section for examples) will help reduce symptoms of gas, bloating, spasm, cramping, and any motility changes by reducing the levels of fermentation done by your infected gut flora.
Commit to the long haul and gut restoration
Sometimes infections are easy to treat and are readily knocked out, and sometimes they are not. Anyone experiencing a frank infection should be prepared for 12 weeks of gut-healing practice (focusing on nutrition, improving digestive fire, supporting the microbiome, healing intestinal integrity and de-stressing the Second Brain) in addition to their antimicrobial therapy (even though antimicrobial therapy may not last that long).
Some folks opt for both conventional and natural antimicrobials, harnessing the best of both worlds. If you take that approach, natural antimicrobials are typically swapped every 3-4 weeks. Taking the time to focus on healing your gut knocks out the infection and improves the health of your digestive tract, making relapse or another infection less likely.
Choose antimicrobials that are appropriate for YOU
Your sensitivity test should be the primary way that you determine what antimicrobials to use, whether they are natural or pharmaceutical. There is good data that demonstrates the efficacy of a variety of plant-based antimicrobials. Grapefruit seed extract, berberine, black walnut, plant tannins, garlic/allicillin, oil of oregano, wormwood and wormseed are examples.
Don’t overlook biofilms. In chronic infections or in those who relapse regularly, biofilms may be present. Biofilms are a mini fortress that the bad guys build over themselves to protect against your immune system and antimicrobial therapy. The interlopers group together and use building blocks from your body (calcium, polysaccharides, even metals) to make their fortifications. [tweet_quote]Plant-based antimicrobials include grapefruit seed extract, black walnut, garlic and oil of oregano[/tweet_quote]
While it makes them tricky to treat, it simply means you need more tools. Specific polysaccharide-busting enzymes like glucoamylase, chitosanase, beta-glucanase, cellulase, hemicellulase and pectinase should be used, along with other specific enzymes like lysozyme, protease and peptidase that have DPP-IV activity. An additional enzyme called serratia peptidase or serrazyme is often used, and the best products will also contain disodium EDTA, which helps remove metal. There are several products on the market that have these enzymes in them, specifically for biofilms. Biofilm busters should be taken at the same time as your antimicrobials to enhance delivery.
Bottom line: The number one rule when considering any type of infection, whether it is candida, another type of yeast or parasites or unhealthy bacteria, or SIBO (small intestine bacterial overgrowth), is to test for it. Stool testing can rule all of these things in or out, minus SIBO, which is a breath test. Do not assume you have an infection and go on an extensive protocol without actually knowing what is going on. Get a test, get the data, and go from there.
Micronutrients and Digestion

Unlike the macronutrients of protein, carbohydrates and fiber, micronutrients are vitamins and minerals that are required by the body is smaller amounts than their macro counterparts.
Micronutrients contribute to all aspects of human health, and you derive them from your diet and supplements.
Your gut plays an important role in micronutrient absorption and assimilation. For example, a compound called intrinsic factor is made by the same cells within your stomach that make acid. Intrinsic factor binds vitamin B12 and allows it to be absorbed into your body.
Iron, folate, magnesium, calcium require adequate stomach acid for their absorption. Chronic use of acid-blocking medications has been associated with increased risk of osteopenia and anemia.
Even your gut flora play their part for the uptake of micronutrients. They help to “humanize” (or make usable) the nutrients that we get from plants. This allows more nutrition to be absorbed into your body.
Micronutrients have a lot to do with digestive function as well. Sodium and potassium help maintain water balance in the bowel (which helps keep you regular), and magnesium is one of the best-known micronutrients to help keep things moving.
Bottom line: Vitamins and minerals are absorbed in a variety of ways in your gastrointestinal system. Ensuring healthy gut flora and balanced digestive “fire” promotes optimal micronutrient status, while acid-blocking medications can be detrimental to it.
How to Eat for Better Digestion

The topic of nutrition can be overwhelming. Mountains of books, blogs and gurus all have their say, often offering conflicting advice and resources. This may sound trite, but finding what works for you is one of the key factors in getting to the root of digestive problems, reducing or banishing symptoms, and looking and feeling your best.
Each of us needs a unique amount of protein, carbohydrates, fat, fiber and water. Ideally, we eat the things that are good for us and reduce symptoms, and decrease the things that give us trouble. When it comes to getting rid of pesky symptoms, there are a few things we must consider.
Problematic and inherently irritating foods should be minimized or reduced. Eating for your condition or symptoms may also be necessary, at least until things have healed up and become more functional – or possibly indefinitely.
Elimination Diet

For those struggling with digestive problems, an elimination-challenge diet is a very useful tool. An elimination-challenge diet, when used with other gut restoration practices (more on that below), can be a game changer.
Eating for your diagnosis can be more subtle and nuanced. For example, there is a lot of research that demonstrates that people who have been diagnosed with IBS or other dysbiosis-based issues benefit from a low FODMAP (Fermentable Oligosaccharide, Disaccharide, Monosaccharide and Polyols) diet. FODMAP is just a fancy acronym to say certain carbohydrates and fibers can be problematic (gas producing, motility changing, pain inducing) for those with an imbalanced microbiome. FODMAPs are found in a wide variety of seemingly random foods. Gluten and dairy are high in FODMAPs, but many healthy – and even classically gut-friendly – foods contain high FODMAPS, like onion, apples, avocado and asparagus.

Take stock of the foods you eat regularly and compare them to the foods that can be inherently irritating or specific to your condition. These are the items you want to target for elimination. Elimination diets can be done with one food at a time or many – it depends on what you are able to handle and commit to.
Elimination diets help you to assess whether a food is truly an issue for you, if it is/was an issue because of something off in your system, or if it’s not an issue at all. It’s important to know so you’re not overly restrictive if you don’t have to be, because that can be pretty miserable.
Typically an elimination is done for 4-6 weeks, in conjunction with other gut-tuning inputs. After that time, if symptoms have significantly improved, a challenge is warranted so you can see how your body responds to the food(s) you have eliminated. Challenges are done one food item at a time, 3-4 days apart.
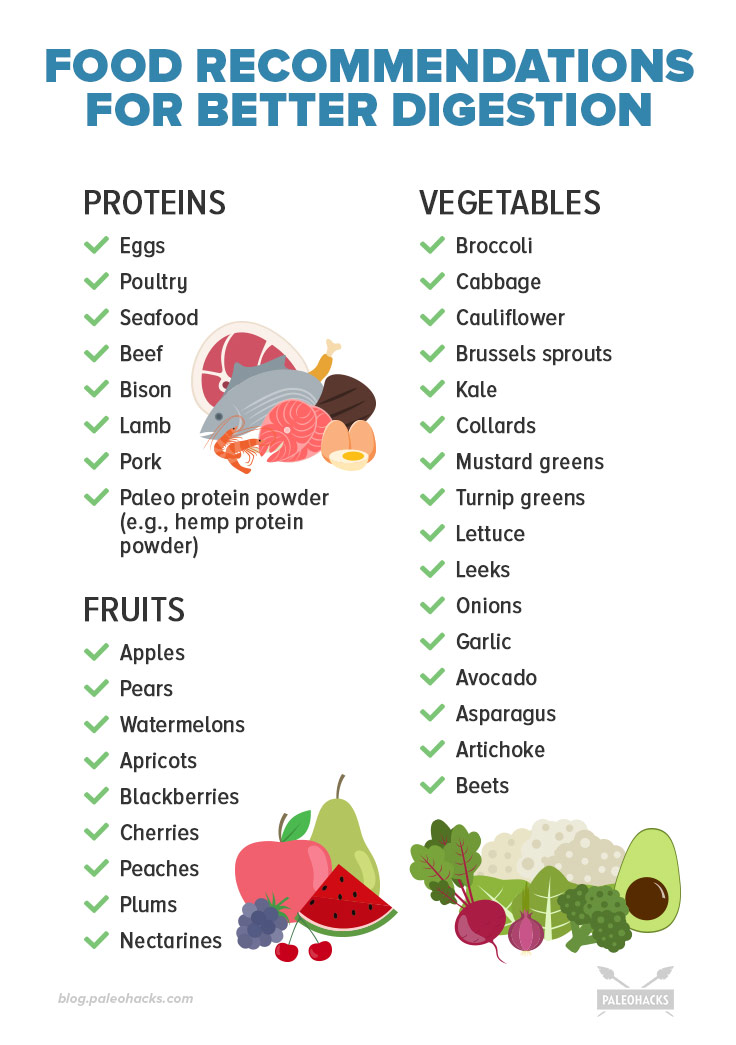
Foods to Eat for Digestive Health
Clearly digestive health is more than just the foods you eliminate. A large part of modern nutrition is the fact that mega-processed foods have displaced the good stuff. Truth is, most of us can handle some junk if our base nutrition is good the majority of the time.
Emphasizing good food on a regular basis is a key strategy in digestive health and wellness. Often, I will coach folks to bring in foods before they start eliminating them. This is particularly powerful for those who feel overwhelmed by, or under committed to, the process.
The most beneficial things to focus on adding into your daily nutrition are high quality protein, vegetables and water. Also included are fruit options. Vegetables and fruits are sources of fiber, antioxidants, vitamins, minerals, polyphenols. There is an enormous amount of variability in the choices available for each of these categories, parlayed with your own unique personal preferences and sensitivities. Play to your strengths and go for what you like rather than trying to force yourself to eat something you don’t like. It’s not fun, and you’ll probably find yourself dropping the food anyway. Our willpower only lasts so long!
Keep in mind that this is a general list, and that there may be items that you don’t like or that your body doesn’t tolerate. You may notice some foods on this list that were included in the problematic foods section. This is not meant to be confusing, but rather to highlight the variability these foods can have on different people. Listen to your body and experience first
Bottom line: Nutrition plays an enormous role in how you feel and look, and your digestion is no exception to that. In fact, many digestive problems are initiated or exacerbated by the foods you may eat, and can be helped by making changes to the diet.
Supplements for Better Digestion

This section could fill a whole book – and indeed it has – but this is a solid list of the most helpful supplements to improve your digestive function and reduce pesky, common symptoms.
Digestive enzymes: Enzymes help you break down proteins, fats and carbohydrates. They will help with a wide variety of symptoms, including gas and bloating, and help improve the consistency and frequency of bowel movements.
Look for a product that contains pepsin, protease, lipase and amylase, and take 1-2 with each meal.
Probiotics: These are the supplemental form of beneficial bacteria, and are highly useful in both constipation and diarrhea, particularly if there is a history of antibiotic use, recent food poisoning or lots of international travel. Probiotics help improve the diversity and strength of your gut flora.
Find a probiotic that contains strains of Lactobacillus and Bifidobacterium. More variety is superior to single strains. In general, doses starting at 10 billion CFUs are well tolerated.
Encapsulated peppermint oil: If you struggle with intestinal pain, cramping and spasm, give encapsulated peppermint oil a try. It helps to reduce spasm, colic and gas pains, but please avoid it if you’ve got heartburn and reflux, for it could make those worse (it relaxes your lower esophageal sphincter, the trap door between the esophagus and the stomach).
Take one capsule after meals.
L-glutamine: Glutamine, the most common amino acid in the human diet, is also the preferential fuel for the cells that line the digestive tract. Beyond nourishment, glutamine also helps these cells to divide, regenerate and repair themselves. This is a must-have for those struggling with intestinal integrity – aka “leaky gut” – issues.
Glutamine has the added benefit of helping with muscle recovery and decreasing muscle soreness for athletes and those who exercise frequently.
A typical dose is 4 grams two to three times daily
Magnesium glycinate: The quintessential natural laxative, magnesium glycinate is the gentlest form on the block, with the extra perks of easing tight muscles, reducing headaches, settling heart palpitations and more. Magnesium, used by the body in over 300 biochemical reactions, is very safe and inexpensive.
Take 450-600mg before bed. The amount can be adjusted up or down based on your own individual response, and keep in mind that if you get loose stool from magnesium supplementation, you should decrease your dose!
Bottom line: The above supplements are helpful and safe, but if you have any questions or concerns or need additional guidance, ask your doctor or competent health care provider.
7-Day Gut-Healing Meal Plan
Sometimes all you need is a little guidance to get focused on changing your health. Here is a 7-day meal plan that can help get your digestion back on track.
Day 1

- Savory Zucchini Pancakes with Bacon and Chives. These are fast, delicious and low-FODMAP. Containing protein, fiber and healthy fats, they will get you off to the right start.
- Paleo Tacos. There are several different options here, all of which contain protein and healthy fats and are low-FODMAP.
- Crock Pot Apple Cider Pork Roast. Cooking a whole roast is great for leftovers or for freezing for future use. Apple cider can be substituted by bone broth.
Day 2

- Easy Baked Avocado and Egg. Emphasis on the easy. This is a great, fast breakfast. If you want to stick to low-FODMAP, make this in muffin tins, ditch the avocado and use bok choy or arugula instead.
- Sweet Potato Gnocchi with Caramelized Brussels Sprouts. This is where it is at for micro nutrition for your gut. Vitamins, minerals, healthy plant compounds and gentle fiber.
- One-Pan Lemon and Herb Chicken. Convenience and flavor reign high in this protein-packed, low-carbohydrate supper.
Day 3

- Almond Flour Pancakes. Containing only three ingredients, these pack a good amount of protein without busting your gut.
- Cajun Chicken Pasta with Light Zucchini Noodles. Low-FODMAP, flavorful and fresh, this recipe will liven your midday meal.
- One-Pan Salmon Dinner with Sweet Potatoes. Salmon is a delicious source of beneficial fatty acids, while sweet potatoes bring a healthy dose of vitamin A.
Day 4

- Caramel Protein Smoothie. The dates add a delicious caramel silkiness to the recipe and happen to be one of those slippery foods – along with bananas – that help the lining of the digestive tract.
- Energizing Power Bowl. This recipe is fast, nutrient-dense and packed with flavor. Add your favorite veggies and enjoy!
- Tortilla-free Steak Wraps. No fuss, high protein and low-FODMAP to make your gut feel good – this one is great for busy nights.
Day 5
- Paleo Cinnamon Raisin Bread. Sounds decadent, but is relatively low-FODMAP and won’t send your blood sugar or your waistline on tilt.
- Taco Salad. This salad is loaded with protein, veggies and flavor and is easily made in bulk to be used for leftovers the next day if you desire!
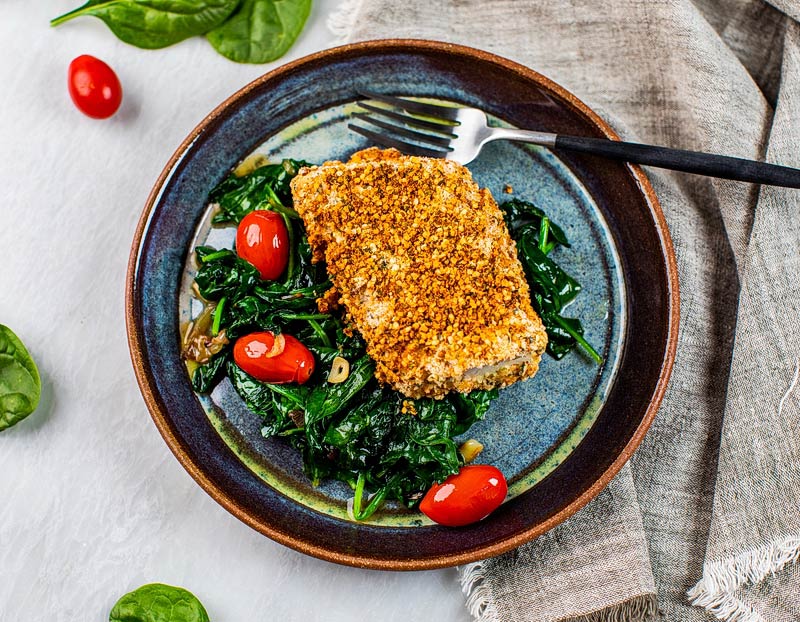
- Baked Cod with Hemp seed Coconut Crust. This gut booster has excellent protein, beneficial fats, and gentle fiber.
Day 6

- Paleo AIP Smoothie. Not just for those with autoimmunity, this is a delicious, clean smoothie full of protein and antioxidants to soothe your gut.
- Paleo Egg Salad. Lovers of egg salad should not skip this dish loaded with protein, healthy fats and brain supportive nutrients.
- Paleo Bacon Burger. Sometimes, you just want a bacon burger, and this cleaned-up version will not disappoint your taste buds or your digestion.
Day 7

- Paleo Egg Bake. This is a great option for those looking to prepare a lot of food at once for convenience. Rich in protein and healthy fats, this flexible recipe will allow you to sub any veggies to your taste and unique sensitivities.
- Pumpkin Turmeric Soup. Scroll down to find the soup recipe and use pumpkin. You may also sub butternut squash or other winter squashes in this recipe. Turmeric is a powerful anti-inflammatory and pumpkin provides gentle fiber and antioxidants for your gut.
- One-Pan Shrimp and Veggie Dinner. Shrimp is a great way to vary your protein intake while getting in beneficial vitamins and minerals too. This easy dish is scrumptious and features mostly low-FODMAP vegetables.
Read This Next: The Ultimate Guide to Perfect Digestion



 How to Make Dairy Free Coconut Yogurt
How to Make Dairy Free Coconut Yogurt









Show Comments